QUT has received a $1M grant to develop technology that improves diagnosis and prediction of coronary artery disease, the leading cause of sudden deaths in Australia, killing an average of two people every hour.
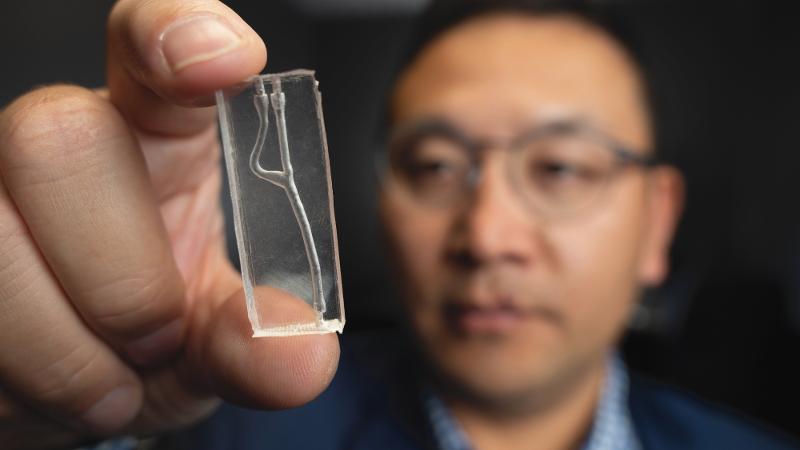
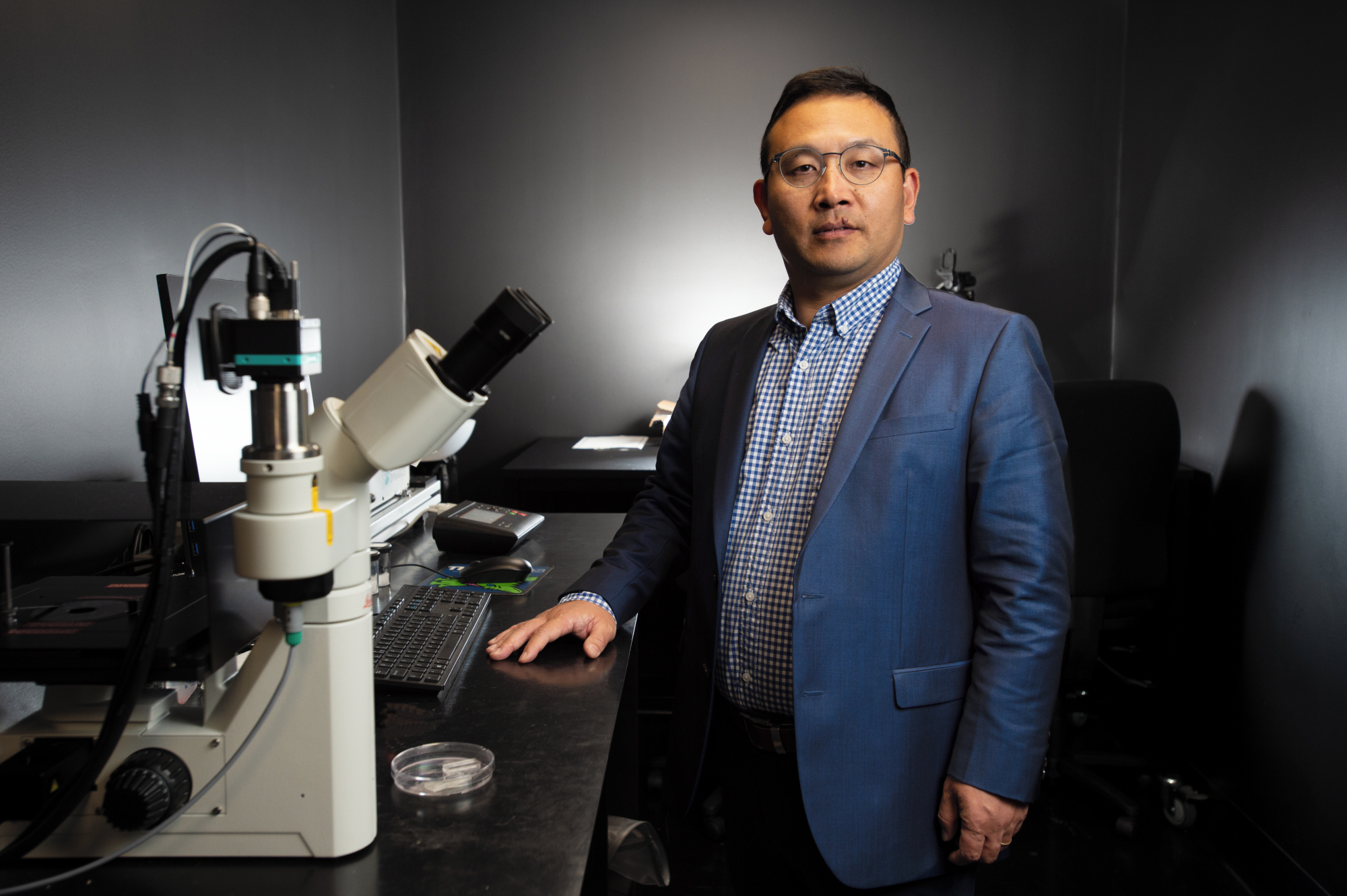
Chief investigator, Professor Zhiyong Li (pictured) from the QUT Centre for Biomedical Technologies and the Faculty of Engineering, School of Mechanical, Medical and Process Engineering, will lead the three-year project funded by the Australian Government Medical Research Future Fund.
He said technologies for predicting acute coronary syndrome – heart attacks – caused by coronary artery disease were still limited despite decades of advancement.
“Most people won’t know they are at risk of heart attack until they have one because they won’t experience symptoms,” Professor Li said.
“The number of heart attacks each year remains high despite enormous efforts to understand plaque formation in arteries and identify at-risk patients.
“But current technology only shows artery narrowing and not the effect on blood flow.”
Cardiovascular diseases cost the Australian health system almost $5B annually, with more than $2.3B attributed to coronary artery or coronary heart disease.
Professor Li said coronary artery disease claimed more lives than any other disease in Australia, killing one person every half hour, and twice as many men compared to women.
“Heart attacks from coronary artery disease are the result of a complex interplay between blood flow and plaque in narrowed arteries,” he said.
“The integration of current and new technologies could enhance diagnosis and allow monitoring of the disease risk to prevent unexpected heart attacks and save people’s lives.”
He said diagnosis was currently made with computerised tomography coronary angiogram (CTCA) - imaging of arteries that supply blood to the heart.
Researchers will develop two new complementary technologies to personalise diagnosis at the point of care - during check-ups or hospital visits.
An algorithm will build a biomechanical model of a patient’s heart and simulate blood flow based on their CTCA data.
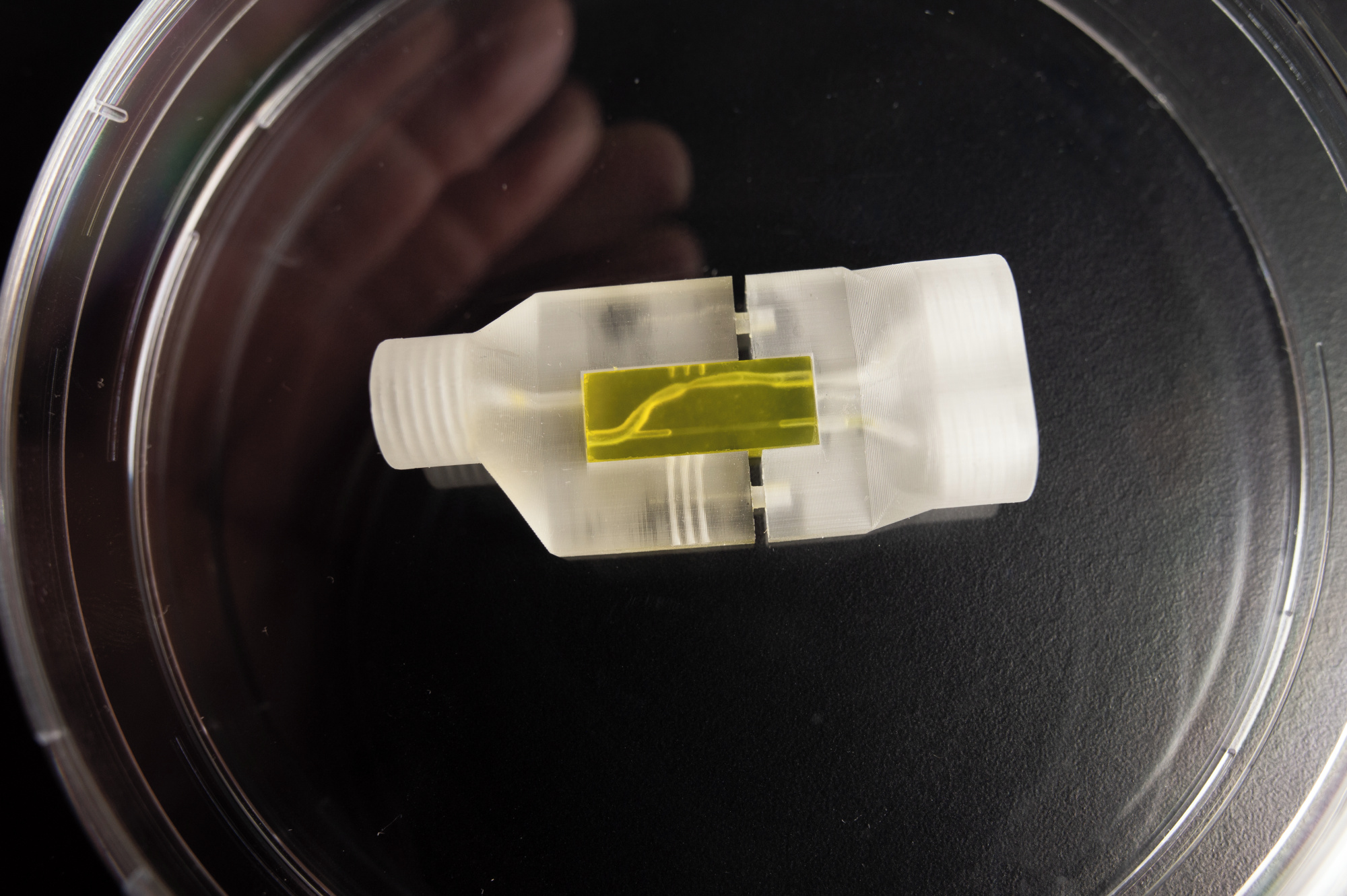
A new blood test will then determine thrombosis risk with a 3D-printed microfluidic chip – a scaled-down replica of a patient’s narrowed artery that only requires a drop of a blood to simulate their likelihood to form clots.
“The new technologies will allow us to mimic both physical and biological conditions of each patient,” Professor Li said.
“If we can identify high risk patients earlier, we can personalise and prioritise their treatment, or monitor them over time for any increase in risk.
“More accurate diagnosis could also help avoid unnecessary surgeries in favour of other interventions, improve health outcomes and relieve pressure on healthcare systems.”
Professor Li said developed technologies would be tested through BioHEART, a large clinical study of people with plaque build-up in arteries, together with fellow chief investigators, Professor Gemma Figtree, Professor Stuart Grieve and Dr Lining Ju, from the University of Sydney.
Among the experts joining Professor Li is world-recognised mathematics and statistics research, Distinguished Professor Kerrie Mengersen from the QUT Centre for Data Science, who has applied her work to other health-related outcomes including breast cancer screening.
Project partners include the Queensland Cardiovascular Group, Brisbane Cardiology Clinic, University of Sydney, and the Princess Alexandra Hospital.
Media contacts
Novella Moncrieff, 07 3138 1150, novella.moncrieff@qut.edu.au
After hours, 0407 585 901 or media@qut.edu.au


